Some people choose to have both fallopian tubes removed as a permanent birth control method or to reduce the risk of ovarian cancer. Scientists have recently discovered that most ovarian cancers likely start as small tumors in the fallopian tubes, not in the ovaries.
What you need to know:
- Salpingectomy involves the removal of one or both fallopian tubes.
- It can be performed to treat an ectopic pregnancy. An ectopic pregnancy occurs when a fertilized egg develops outside the uterus, such as when it implants in the fallopian tubes.
- Bilateral salpingectomy involves the removal of both fallopian tubes. This is a permanent form of birth control for individuals who do not want any more pregnancies. A person can become pregnant with just one fallopian tube.
- Salpingectomy may reduce the risk of cancer of the fallopian tubes, ovary, and peritoneum (the membrane surrounding the abdominal organs).
Salpingectomy to prevent cancer of the fallopian tubes, ovary, or peritoneum can be performed during another abdominal procedure and is recommended for individuals who do not wish for future pregnancies.
What is a salpingectomy?
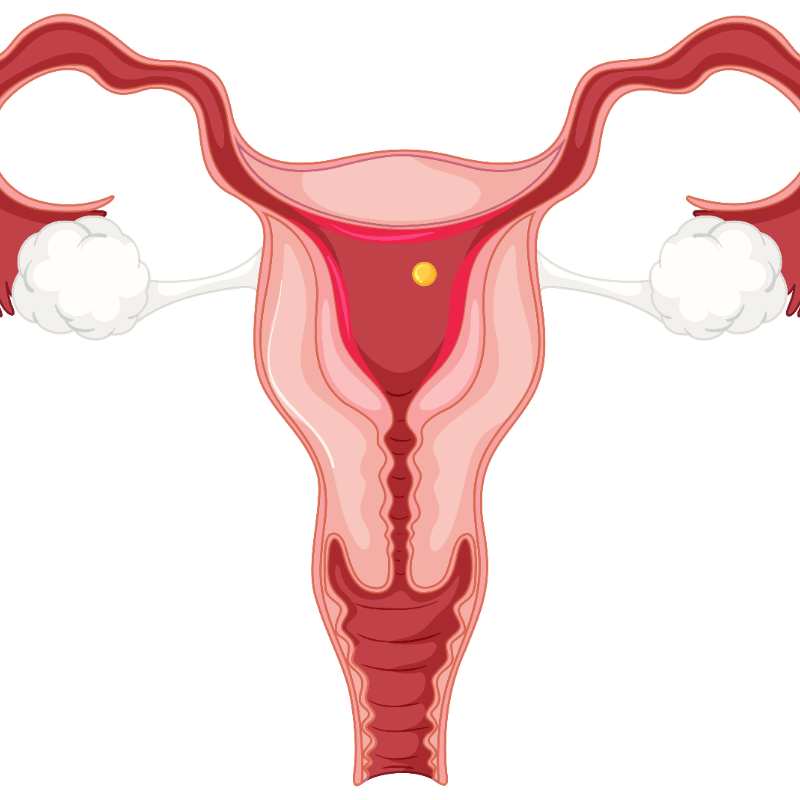
Salpingectomy means excision of the fallopian tubes. The fallopian tubes are hollow structures through which eggs pass from the ovaries to the uterus. The term can refer to procedures that completely remove one or both fallopian tubes or that only remove parts of the fallopian tubes.
Types of salpingectomy
The decision to remove either totally or partially a fallopian tube depends on why the procedure is being performed, the age and health of the patient, and their concerns about fertility.
- Salpingo-oophorectomy is the removal of the fallopian tubes and the ovary. It can be unilateral (removal of one tube and one ovary, usually from the same side) or bilateral (removal of both tubes and one or both ovaries).
When both ovaries are removed, the person is in menopause, because the ovaries produce hormones, and their removal stops this production. Bilateral oophorectomy performed at a young age has been shown to increase the risk of heart disease, osteoporosis, and other conditions. When one ovary is removed, hormone production from a single ovary is sufficient. - Ovarian-conserving salpingectomy means that the person maintains their estrogen and other hormone levels because the ovaries are left in place: only the fallopian tubes are removed.
- Opportunistic salpingectomy is the elective removal of both fallopian tubes during another abdominal surgical procedure (such as gallbladder surgery, hernia repair, cesarean section, or hysterectomy) to prevent cancer of the fallopian tubes, ovary, or peritoneum.
Why is a salpingectomy recommended?
There are several reasons why a doctor may recommend a salpingectomy to treat a patient. Because surgery can affect fertility and cancer prevention, it is important to communicate with the doctor and understand the impact of the procedure.
Ectopic pregnancy
An ectopic pregnancy is a complication of pregnancy that involves a fertilized egg developing outside the uterus. An ectopic pregnancy that originates in a fallopian tube cannot lead to the birth of a baby and may eventually cause the tube to rupture, potentially leading to life-threatening bleeding. In some cases, an ectopic pregnancy constitutes a surgical emergency.
A salpingectomy may be necessary to completely or partially remove the affected fallopian tube to manage an ectopic pregnancy. The gynecologist/obstetrician works with the patient to preserve her fertility whenever possible.
Permanent birth control
Salpingectomy and tubal ligation are two permanent contraceptive methods. These methods are chosen for health reasons or personal preference.
While tubal ligation involves using a ring or clip to close the fallopian tubes, salpingectomy cuts the fallopian tubes by removing a central segment (partial salpingectomy) or separates the fallopian tubes from the uterus and completely removes them (complete salpingectomy).
While both tubal ligation and complete salpingectomy are very effective at preventing pregnancy, complete salpingectomy is the most effective as a contraceptive and provides the greatest benefit in terms of cancer prevention.
Bilateral salpingectomy for cancer prevention.
Ovarian cancer is the most dangerous of all gynecological cancers because it is usually diagnosed at an advanced stage, and the chances of curative treatment are low.
Shih explains that recent research shows that some forms of ovarian cancer do not start in the ovary itself, but rather in the finger-like projections at the end of the fallopian tubes, called fimbriae. Cancer cells that grow in this area spread to the ovary and the peritoneum, the membrane that surrounds the abdominal organs. Primary extra-ovarian peritoneal carcinoma (EPC) is a form of cancer that affects the peritoneum and can originate from cancerous cells in the fallopian tubes.
Since many ovarian cancers develop in the fallopian tubes, we can reduce the risk of ovarian cancer by removing the fallopian tubes in individuals who do not wish to become pregnant.
The risk of ovarian cancer may be higher if the person has already had breast cancer or if their family has a history of breast, ovarian, pancreatic, or colon cancer. Genetic testing may be recommended.
Individuals with hereditary cancer risk, including those with mutations in the BRCA1 and BRCA2 genes or associated with Lynch syndrome, have a lifetime risk exceeding 1% or 2% for developing ovarian cancer. For them, the removal of the fallopian tubes and ovaries, generally between the ages of 35 and 50, depending on the genetic mutation, is the recommended standard of care. This will continue until we have the results from prospective research in the coming years.
Opportunistic salpingectomy for cancer prevention
Even individuals without known risk factors for ovarian cancer may benefit from the removal of the fallopian tubes.
Salpingectomy reduces the risk of ovarian cancer in all individuals. It is essential to understand that individuals at average risk of ovarian cancer (those whose hereditary risk is unknown) may benefit from salpingectomy for ovarian cancer prevention once they no longer wish to have children.
Salpingectomy to reduce the risk of ovarian cancer can be performed at the same time as another planned abdominal surgery, for example, at the same time as gallbladder removal or hernia surgery. This is called opportunistic salpingectomy, and it takes advantage of the opportunity to remove both fallopian tubes during another abdominal surgery to prevent ovarian, fallopian tube, and peritoneal cancer.
Opportunistic salpingectomy is recommended for cancer prevention in individuals who do not have hereditary risk for ovarian cancer due to the BRCA gene or other genetic mutations.
Researchers are studying whether the same risk reduction can be achieved simply by removing the fallopian tubes and leaving the ovaries in place in individuals who have a genetic predisposition due to genetic mutations like BRCA. But for now, opportunistic salpingectomy is recommended for individuals with an average risk of ovarian cancer (1 to 2% lifetime risk).
Currently, we do not have an effective screening test for ovarian cancer. Pap tests cannot detect ovarian cancer. However, future research hopes to identify subtle changes in cells collected during Pap tests, which could help identify at-risk individuals so they can opt for surgery sooner to reduce risk.
Salpingectomy: what to expect
Laparoscopic salpingectomy can be performed on the same day in a hospital or surgical center.
Laparoscopy means that the surgeon performs the procedure through small incisions (less than half an inch) in the abdomen. Same-day means that you will not need to be admitted to the hospital and will be able to go home on the day of the operation. It is important to plan a ride home after a salpingectomy because the procedure typically requires general anesthesia.
In some cases, a procedure called mini-laparotomy may be used to perform a salpingectomy. The surgeon accesses the fallopian tubes through a small incision in the pubic region. In this case, the individual may choose to receive spinal anesthesia instead of general anesthesia. Spinal anesthesia is a nerve block that eliminates sensation in the lower abdomen. It is commonly used for cesarean sections.
Removing the fallopian tubes during another abdominal procedure is usually straightforward. When salpingectomy is added to another surgical procedure in the abdomen, it typically takes only a few minutes and does not add significant risk to the surgical experience. Salpingectomy can be performed at the same time as an endoscopic abdominal procedure (laparoscopic or robotic) or an open abdominal procedure (a single long incision in the abdomen).
Salpingectomy: What Happens?
Salpingectomy performed with a laparoscope typically requires three small incisions, one near the navel and the others in the lower abdomen (belly).
The surgeon locates the fallopian tubes and examines them along their entire length. Using surgical instruments such as forceps, the surgeon takes the tube and separates it from the ovary and uterus, often using an energy device to seal and divide the small vessels along the way.
Recovering from a salpingectomy
- It is important to follow the surgeon's instructions after the procedure. Talk to your doctor about when it is safe to start having sexual intercourse again.
- Salpingectomy procedures for contraception are effective immediately. You will not need to use other contraceptive methods once you have recovered from the procedure. However, the procedure does not protect against sexually transmitted infections, so condoms should continue to be used to prevent them.
Recovery usually takes one to three weeks after the procedure and may take longer after a cesarean section or childbirth.
Risks and complications of salpingectomy.
Laparoscopic salpingectomy has few risks. In rare cases, patients may experience the following complications after surgery:
- Bleeding
- Hernia
- Accidental injury to abdominal organs
- Infection
- Scarring
- Chronic pain
- Need for a longer incision (called laparotomy)
Can you get pregnant after a salpingectomy?
Contrary to popular belief, women can still conceive after a salpingectomy, but the process is somewhat different.
After a salpingectomy, the egg released during ovulation goes directly into the pelvic cavity. In the absence of fallopian tubes, conception occurs when sperm fertilizes the egg in this pelvic space. However, the fertilized egg must implant in the uterus for a viable pregnancy to occur. It is important to note that the absence of fallopian tubes increases the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus, usually in the abdominal cavity. Ectopic pregnancies are not viable and pose serious health risks to the woman.
For women who wish to become pregnant after a salpingectomy, assisted reproductive techniques (ART), such as in vitro fertilization (IVF) or egg donation, become attractive options. IVF involves collecting eggs directly from the ovaries, fertilizing them with sperm in the laboratory, and transferring the resulting embryos to the uterus. This method bypasses the need for fallopian tubes and increases the chances of a successful pregnancy. In cases where a woman's eggs are not viable, egg donation offers an alternative using eggs from a donor, which often results in successful pregnancies.
It is crucial for women considering pregnancy after a salpingectomy to consult fertility specialists. They can assess individual circumstances, discuss available options, and create a personalized plan. Factors such as age, overall health, and the reason for the salpingectomy will influence the most appropriate approach to maximize the chances of achieving a healthy pregnancy. Although salpingectomy alters the natural reproductive process, advances in reproductive medicine, including egg donation, allow many women to realize their dream of becoming mothers.
Our experts are ready to examine your case history, clarify your choices, and address every question you have.
Don't wait to make informed decisions – your personalized guidance awaits!
- Spain (España)+34
- France (La France)+33
- Italy (Italia)+39
- United Kingdom+44
- United States+1
- Belgium (België)+32
- Switzerland (Schweiz/Suisse)+41
- Germany (Deutschland)+49
- Netherlands (Nederland)+31
- Afghanistan (افغانستان)+93
- Albania (Shqipëri)+355
- Algeria (الجزائر)+213
- American Samoa+1
- Andorra+376
- Angola+244
- Anguilla+1
- Antigua and Barbuda+1
- Argentina+54
- Armenia (Հայաստան)+374
- Aruba+297
- Ascension Island+247
- Australia+61
- Austria (Österreich)+43
- Azerbaijan (Azərbaycan)+994
- Bahamas+1
- Bahrain (البحرين)+973
- Bangladesh (বাংলাদেশ)+880
- Barbados+1
- Belarus (Беларусь)+375
- Belize+501
- Benin (Bénin)+229
- Bermuda+1
- Bhutan (འབྲུག)+975
- Bolivia+591
- Bosnia and Herzegovina (Босна и Херцеговина)+387
- Botswana+267
- Brazil (Brasil)+55
- British Indian Ocean Territory+246
- British Virgin Islands+1
- Brunei+673
- Bulgaria (България)+359
- Burkina Faso+226
- Burundi (Uburundi)+257
- Cambodia (កម្ពុជា)+855
- Cameroon (Cameroun)+237
- Canada+1
- Cape Verde (Kabu Verdi)+238
- Caribbean Netherlands+599
- Cayman Islands+1
- Central African Republic (République centrafricaine)+236
- Chad (Tchad)+235
- Chile+56
- China (中国)+86
- Christmas Island+61
- Cocos (Keeling) Islands+61
- Colombia+57
- Comoros (جزر القمر)+269
- Congo (DRC) (Jamhuri ya Kidemokrasia ya Kongo)+243
- Congo (Republic) (Congo-Brazzaville)+242
- Cook Islands+682
- Costa Rica+506
- Côte d’Ivoire+225
- Croatia (Hrvatska)+385
- Cuba+53
- Curaçao+599
- Cyprus (Κύπρος)+357
- Czech Republic (Česká republika)+420
- Denmark (Danmark)+45
- Djibouti+253
- Dominica+1
- Dominican Republic (República Dominicana)+1
- Ecuador+593
- Egypt (مصر)+20
- El Salvador+503
- Equatorial Guinea (Guinea Ecuatorial)+240
- Eritrea+291
- Estonia (Eesti)+372
- Eswatini+268
- Ethiopia+251
- Falkland Islands (Islas Malvinas)+500
- Faroe Islands (Føroyar)+298
- Fiji+679
- Finland (Suomi)+358
- French Guiana (Guyane française)+594
- French Polynesia (Polynésie française)+689
- Gabon+241
- Gambia+220
- Georgia (საქართველო)+995
- Ghana (Gaana)+233
- Gibraltar+350
- Greece (Ελλάδα)+30
- Greenland (Kalaallit Nunaat)+299
- Grenada+1
- Guadeloupe+590
- Guam+1
- Guatemala+502
- Guernsey+44
- Guinea (Guinée)+224
- Guinea-Bissau (Guiné Bissau)+245
- Guyana+592
- Haiti+509
- Honduras+504
- Hong Kong (香港)+852
- Hungary (Magyarország)+36
- Iceland (Ísland)+354
- India (भारत)+91
- Indonesia+62
- Iran (ایران)+98
- Iraq (العراق)+964
- Ireland+353
- Isle of Man+44
- Israel (ישראל)+972
- Italy (Italia)+39
- Jamaica+1
- Japan (日本)+81
- Jersey+44
- Jordan (الأردن)+962
- Kazakhstan (Казахстан)+7
- Kenya+254
- Kiribati+686
- Kosovo+383
- Kuwait (الكويت)+965
- Kyrgyzstan (Кыргызстан)+996
- Laos (ລາວ)+856
- Latvia (Latvija)+371
- Lebanon (لبنان)+961
- Lesotho+266
- Liberia+231
- Libya (ليبيا)+218
- Liechtenstein+423
- Lithuania (Lietuva)+370
- Luxembourg+352
- Macau (澳門)+853
- North Macedonia (Македонија)+389
- Madagascar (Madagasikara)+261
- Malawi+265
- Malaysia+60
- Maldives+960
- Mali+223
- Malta+356
- Marshall Islands+692
- Martinique+596
- Mauritania (موريتانيا)+222
- Mauritius (Moris)+230
- Mayotte+262
- Mexico (México)+52
- Micronesia+691
- Moldova (Republica Moldova)+373
- Monaco+377
- Mongolia (Монгол)+976
- Montenegro (Crna Gora)+382
- Montserrat+1
- Morocco (المغرب)+212
- Mozambique (Moçambique)+258
- Myanmar (Burma) (မြန်မာ)+95
- Namibia (Namibië)+264
- Nauru+674
- Nepal (नेपाल)+977
- New Caledonia (Nouvelle-Calédonie)+687
- New Zealand+64
- Nicaragua+505
- Niger (Nijar)+227
- Nigeria+234
- Niue+683
- Norfolk Island+672
- North Korea (조선 민주주의 인민 공화국)+850
- Northern Mariana Islands+1
- Norway (Norge)+47
- Oman (عُمان)+968
- Pakistan (پاکستان)+92
- Palau+680
- Palestine (فلسطين)+970
- Panama (Panamá)+507
- Papua New Guinea+675
- Paraguay+595
- Peru (Perú)+51
- Philippines+63
- Poland (Polska)+48
- Portugal+351
- Puerto Rico+1
- Qatar (قطر)+974
- Réunion (La Réunion)+262
- Romania (România)+40
- Russia (Россия)+7
- Rwanda+250
- Saint Barthélemy+590
- Saint Helena+290
- Saint Kitts and Nevis+1
- Saint Lucia+1
- Saint Martin (Saint-Martin (partie française))+590
- Saint Pierre and Miquelon (Saint-Pierre-et-Miquelon)+508
- Saint Vincent and the Grenadines+1
- Samoa+685
- San Marino+378
- São Tomé and Príncipe (São Tomé e Príncipe)+239
- Saudi Arabia (المملكة العربية السعودية)+966
- Senegal (Sénégal)+221
- Serbia (Србија)+381
- Seychelles+248
- Sierra Leone+232
- Singapore+65
- Sint Maarten+1
- Slovakia (Slovensko)+421
- Slovenia (Slovenija)+386
- Solomon Islands+677
- Somalia (Soomaaliya)+252
- South Africa+27
- South Korea (대한민국)+82
- South Sudan (جنوب السودان)+211
- Spain (España)+34
- Sri Lanka (ශ්රී ලංකාව)+94
- Sudan (السودان)+249
- Suriname+597
- Svalbard and Jan Mayen+47
- Sweden (Sverige)+46
- Syria (سوريا)+963
- Taiwan (台灣)+886
- Tajikistan+992
- Tanzania+255
- Thailand (ไทย)+66
- Timor-Leste+670
- Togo+228
- Tokelau+690
- Tonga+676
- Trinidad and Tobago+1
- Tunisia (تونس)+216
- Turkey (Türkiye)+90
- Turkmenistan+993
- Turks and Caicos Islands+1
- Tuvalu+688
- U.S. Virgin Islands+1
- Uganda+256
- Ukraine (Україна)+380
- United Arab Emirates (الإمارات العربية المتحدة)+971
- Uruguay+598
- Uzbekistan (Oʻzbekiston)+998
- Vanuatu+678
- Vatican City (Città del Vaticano)+39
- Venezuela+58
- Vietnam (Việt Nam)+84
- Wallis and Futuna (Wallis-et-Futuna)+681
- Western Sahara (الصحراء الغربية)+212
- Yemen (اليمن)+967
- Zambia+260
- Zimbabwe+263
- Åland Islands+358
Visit our clinic
Location
Call us now
Leave a message










